The Role of VR in Gynecological and OB-GYN Specialty Training

Consider this: how often have medical students complained about not being able to visualize the spatial relationships between organs during a gynecological lecture?
This is a real challenge and proves the necessity of finding different solutions. Or was there perhaps limited access to cadaveric material or live patients for practical training?
Now picture yourself in a place where human anatomy becomes fleshed out, where all the inner workings of the female reproductive system become open to the safe examination of all involved.
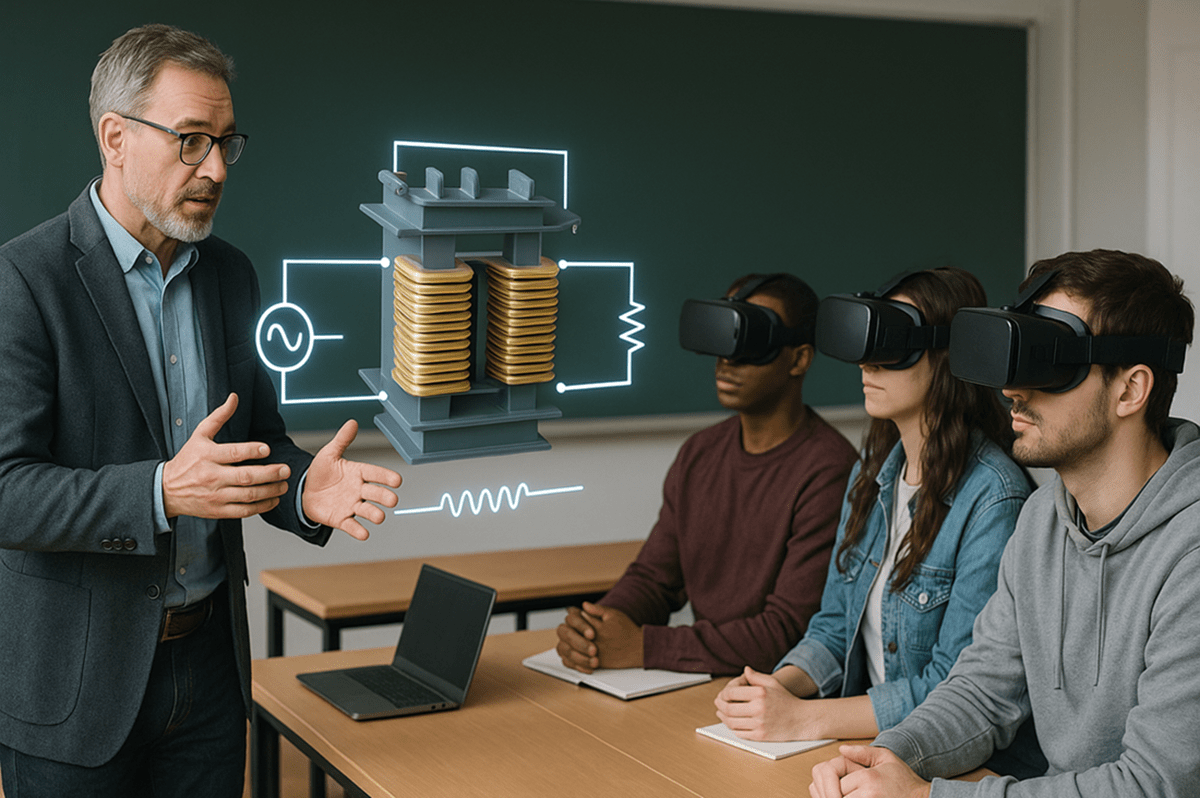
A study involving 117 medical students revealed a 24.9% improvement in knowledge scores when utilizing VR for training compared to traditional manikin-based methods.
In this blog, virtual reality (VR) technology is explored, and how it is changing the way gynecology training is delivered, making it more interactive and effective.
Let’s get started.
Challenges With Traditional Gynaecological Training
Even though educators all over the world have been trying their best, most parts of gynecology education are still based on textbooks, lectures, and a few hours of hands-on experience.
Although these are good basic methods, for clinical judgment they lack the interactive elements that are needed to develop. This is why colleges need VR education, so that the gaps in teaching are addressed and the learning outcomes increase manifold.
Bridging the Gap with Virtual Reality
The European Journal of Midwifery conducted a study that indicated students who were subjected to immersive VR environments displayed improved spatial learning and anatomical knowledge more than traditional methods.

Let's look at the exact benefits provided by VR to the gynecology field :
Enhanced Spatial Reasoning
The problems of space and time for gynecology anatomy training in VR are addressed by trainees interacting with 3D models of the female reproductive system.
For example, trainees can run through a laparoscopic hysterectomy and pick up valuable experience while simultaneously relieving themselves of the pressure of the real thing.
This is happening at Central Michigan University. The university is using a highly realistic VR simulator of laparoscopic surgeries, including hysterectomies.
The simulator offers haptic feedback, allowing trainees to 'feel' the tissue when they manipulate it, and simulating a real operating room environment. This is one of the many instances of VR changing healthcare with innovative solutions.
Detailed Visualisation
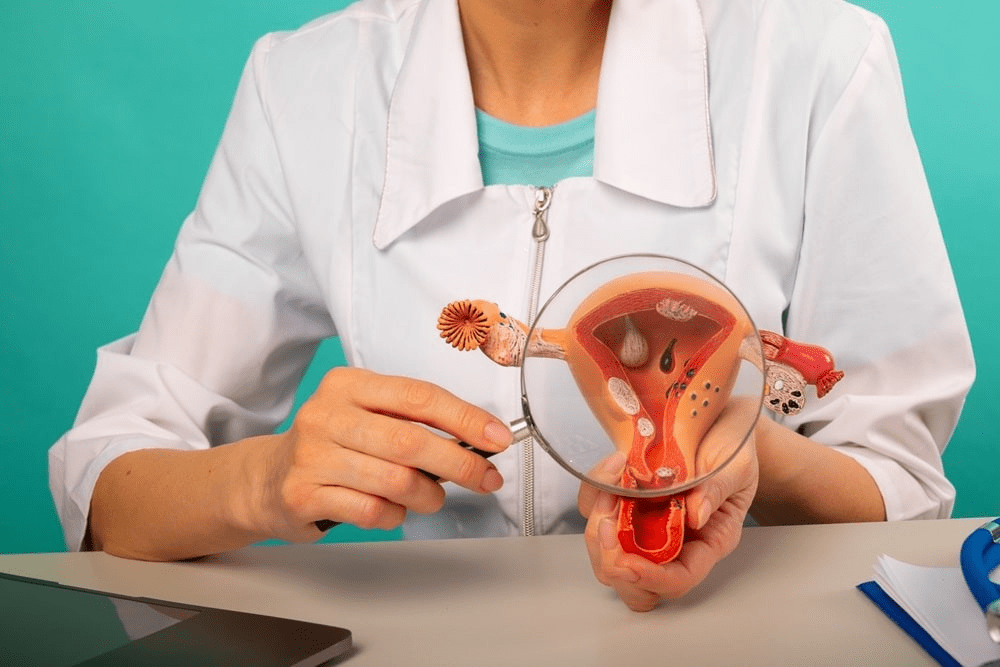
One of the several advantages of immersive technology in medicine is the ability to use detailed visualization of anatomical structures. With 3D models of body parts facilitated by immersive VR platforms, students can rotate them, zoom, and pivot in on certain areas to go deeper than a textbook can.
Risk-free Simulation
Traditional surgical training comes with significant risks for both the educator and the student. Researchers create hands-on VR learning modules that allow trainees to practice procedures repeatedly without putting patient safety at risk.
For example, a virtual pelvic cavity lends the medical student an environment where she can navigate through it while practicing diagnostic techniques similar to what she would also do in reality, and identify the anatomical structures.
This transformation of medical education in VR will keep morale high so that, when they enter the operating room, they’ll be prepared.
Precision and Repetition
In gynecology, procedures need high precision. VR permits repetitive practice, which enhances muscle memory and procedure accuracy.
By rehearsing complex maneuvers until they master them, residents' confidence levels skyrocket when it comes time to perform the surgery for real.
According to a study by the University of Maryland, VR increased learning retention by 10 percent for 40 % of the audience. This stresses VR’s principle of the “Cognitive Load Theory,” which posits that extraneous load has to be removed for more retention of knowledge by the learner.
Global Accessibility
VR technology is also democratizing access to good-quality education. Students can learn from anywhere with VR-enabled gynecology labs implemented by institutions that bring the world closer.
 Get the App from Meta Store: Download Now
Get the App from Meta Store: Download Now
With training now accessible remotely to a student in any part of the world as reliably as training that a student could receive at a famous university, this is not innovation; this is empowerment.
Use Cases of VR Technology in Gynecological Training
Several educational institutions have successfully integrated VR applications in medical education in the field of gynecology.
NewYork-Presbyterian Hospital : A VR-based laparoscopic simulation platform that improved residents' surgical skills and confidence levels significantly was implemented.
University of South Florida, College of Medicine : VR simulations used for hysteroscopic myomectomy training yielded comparable results to traditional training methods but with better reproducibility.
Western Norway University of Applied Sciences: The educators have implemented VR in gynecology training by using immersive simulations to enhance students' understanding of female pelvic anatomy, allowing them to explore and interact with 3D models.
Conclusion
However, the integration of virtual reality in gynecological training is not an improvement but rather a significant change in the way in which we train future doctors. Embracing immersive technologies is the key to enabling the means by which educators can create a better-prepared student for real-world challenges, resulting in overall better patient care.
Therefore, as we look at the future, educational institutions should think about applying these creative solutions. They could have far-reaching effects on learning and also improve the way you care for your patients.
.png)
.png)

.png)